
Sport at low temperatures
FIS Medical Committee Educational Series
Fri, Dec 14, 2007 - By Inggard Lereim
FIS Medical Committee Educational Series
Professor MD PhD Inggard Lereim
Vice-Chairmen of the FIS Medical Committee
Sport at low temperatures
Prevention of cold injuries in snow sports
Introduction
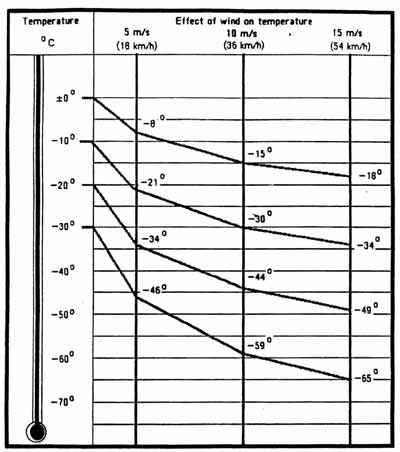
In earlier times, snow sport competitions were held in all types of weather, and little attention was paid to weather conditions. Very few competitions were abandoned because of low temperature. The majority of athletes who participated in winter sports lived in cold countries and worked outdoors and were acclimatised to cold. In addition, little consideration was given to the effect of wind on temperature. We are now very aware that the wind-chill effect should also be taken into account. For example, a wind of 5m/s i.e.18 km/hr will effectively reduce the ambient temperature from 0 to minus 8 degrees C, one of 15 m/s i.e.54 km/hr will reduce it from 0 to minus 18 degrees C.
Nowadays many more athletes train outdoors all year round, including cyclists, marathon runners and others including those participating in winter sports.
Advances in technology have produced changes in quality and style of sportswear which whilst increasing speed may not always provide adequate protection against the cold.
There have been improvements in equipment and in skating technique in skiing, and faster tracks have also resulted in faster times. The resulting chilling effect of the wind can thus lead to a higher incidence of cold injuries and increased susceptibility to diseases. This has stimulated research in this field by medical doctors in different specialities, and by physiologists and trainers. In the following chapters a review of these studies and experiences from ski sport is presented. (1-19).
Even at times when global warming up is looked upon as one of the great threats to the future of snow sports we must not forget the danger of hypothermia in sport.
Hypothermia
A warm up period is essential before any training session or competition. Large muscle groups are activated, e.g. in jogging, to raise the body temperature from 37oC to 38-39oC.
At this temperature oxygen transport is more efficient. The body’s first priority is to maintain an adequate body core temperature when exercising in the cold. Due to the temperature difference there is a much greater loss of body heat to the environment, and so an adequate warm up session is essential to maintain the ability to perform at a high technical level. When the body core temperature drops the athlete’s performance suffers as a result. In severe cold there is first a marked vasoconstriction of the vessels to the skin and superficial parts of the body followed by reduced blood flow to the muscles and tendons.
The effect of hypothermia on different organs
The heart
Moderate hypothermia of 35 degrees C initially stimulates the cardiovascular system, leading to peripheral vasoconstriction, tachycardia and rise in blood pressure. When frank hypothermia occurs, there is a fall in blood pressure, slowing of the pulse, i.e. bradycardia, reflecting myocardial depression. (7,8). Cardiac arrhythmias are most likely to occur at temperatures between 26 and 29 degrees C. As the temperature falls below this the bradycardia may be replaced by atrial fibrillation, atrial flutter, ventricular fibrillation and /or cardiac arrest.
Ventricular fibrillation is probably the commonest cause of death in accidental hypothermia. Cardiac arrhythmias may be associated with heart failure or oedema of the lung.
When rewarming a patient with severe hypothermia, there is an increased risk of cardiac arrhythmia when the patient’s core temperature is between 26 and 29 degrees C (11,16). A defibrillator is an essential piece of equipment to deal with the cardiac arrhythmias during the warm up period. At a body temperature below 20 degrees C cardiac arrest often occurs without rhythm disturbances.
Kidney
Hypothermia may lead to impaired renal function. It usually occurs at a later stage after cardiac failure. It is accompanied by raised blood urea and creatinine. Proteinuria may occur, which in some cases may be severe enough to give peripheral oedema. Haematuria or even haemoglobinuria may occur; both are signs of severe renal damage that is likely to necessitate special treatment, notably dialysis. Disturbances in the balance of electrolytes may occur and may lead to increased risk of other complications such as arrhythmias, independent of the present body core temperature (see above, heart). Great attention must be paid to renal function in the post initial and follow up stage of hypothermia (10,16,17).
Liver
In the more severe cases of hypothermia signs of reduced liver function may be seen, both clinically and in laboratory tests. In the final stages, liver necrosis may occur.
The liver enzymes will be elevated and there is an associated hypoproteinaemia which will increase the risk of oedema. Jaundice will develop due to the elevated bilirubin. This will necessitate a long period of hospitalisation and convalescence.
Like some of the renal complications, the liver symptoms are seen in the post initial and later stages. A follow up with adequate liver function tests during the whole in-patient period and afterwards is essential. A strict regime as to the restart of training must be followed.
Pancreas
Severe hypothermia may cause pancreatic necrosis or haemorrhagic pancreatitis. This is an extremely severe complication of hypothermia and may be fatal. A mortality rate of between 70% and 85% has been reported in hypothermic patients with haemorrhagic pancreatitis. Calcium values in the serum may fall causing cramps. Milder cold injury may cause diabetes.
Pancreatic complications will also require intensive care and long hospitalisation. A close follow up by qualified doctors over many months is necessary, and serum values must return to normal before the patient may return to full activity.
Brain
Mild hypothermia increases the tolerance of the brain to hypoxia. However below 34 degrees C pathological changes occur. Cerebral oedema with increased intracranial pressure is associated with diminished awareness. The patient feels comfortable and there is an absence of pain.
With increasing cerebral hypothermia, slurring of the speech occurs, and movement of the limbs are slow and poorly coordinated with depressed reflexes. Focal paralysis or sensory loss has also been reported. This is probably the result of haemorrhages in the brain which may cause temporary or permanent loss of function. (1,2,6,11,13,18)
The patient may become unconscious, go into coma and die. This stage is rare in sports events. The early signs of diminished awareness should be looked for by the responsible physician. Hospitalisation may be necessary even at the milder stage of general hypothermia if central nervous symptoms are apparent.
Airways
Upper respiratory infections and bronchitis are common complications of athletic training and competition in cold climate. Cold may also precipitate exercise-induced asthma. This may cause considerable problems for competitors in endurance sports such as cross country, Nordic combined, biathlon etc. In recent decades many athletes at international level have suffered from exercise induced asthma and repeated infective diseases in the airways. The potential for inappropriate use of beta agonists (these are on the WADA list of prohibited substances) is well known. The necessary testing and documentation by specialists in airways diseases has been integral to the job of team physicians and antidoping specialists.
Cold protective masks are worn by many skiers, skaters and even cyclists to enable them to train for a longer period of time than was possible before their introduction. The disadvantage of this equipment is the increased airways resistance and increased dead space which makes it difficult to train intensively for long periods.
Respiratory tract infections should be seen and diagnosed by a doctor as early as possible and the appropriate treatment implemented. It is important to emphasise that no athlete should train or compete if she/he has an infection. A premature return to training may result in prolonged fatigue and may also contribute to the development of a regular overtraining reaction. Consideration of these factors is of utmost importance when training at high altitude. Many problems of this nature have been seen in international teams in recent years.
The athletes, as well as the trainers and doctors, must learn to be patient. (3,4,5.10,12,14,19).
Cold allergy
Some athletes may develop antibodies against the cold; this may also provoke exercise induced asthma in susceptible subjects, with increase in bronchial spasm and fall in FEV1.
Among athletes in endurance sports a fair tolerance to cold climate may be seen for many years, followed by respiratory problems at a later stage of their career. Such complications are more rarely seen in athletes born in areas with cold climate. A gradual adaptation by increasing activity over years may the explanation for this higher tolerance. A learned respect for the dangers of the cold may also contribute.
Prevention of infection by cold, in general
One of the most important preventative actions is the wearing of suitable clothing which should consist of inner insulating layers and an outer windproof layer to protect against the wind.
Training periods should be shorter when the temperatures are low. The athlete should not stand around in wet clothing, but should have a warm shower and change into dry clothes.
Press conferences during Olympic Games, World Championships and other events where the press is present should be brief, and should be held after the athlete has changed her/his clothing. Many athletes now change some of their clothing immediately after crossing the finish line, even though out of doors and still in cold surroundings. But this is normally quite quick and is better than staying around in wet clothes.
Inadequate heating and ventilation of waiting room in the doping control station may increase the risk of mild hypothermia and predispose to infection. For this reason the IOC MC in 1993 created a basic demand for such facilities, including proper heating, ventilation and access to shower.
Eye
The eye is one of the most vulnerable organs. Published studies reveal that the cornea and conjunctiva are the most frequently injured. Oedema of the cornea is followed by ulceration and infection. The patient complains of a red painful eye with excessive lachrymation and photophobia. The athlete may think he/she has developed snow blindness.
Lesions of the conjunctiva or sclera may also occur, with similar symptoms, but they are not as common as those occurring in the cornea.
Prevention:
Any snow or ice that is in contact with the eye must be removed. Frequent closing of the eyes will protect and keep the cornea warm, but if the eyelashes are frozen this will not be possible. As a result, the commonest place for lesions is in the middle of the cornea.
Protective glasses should be worn, but the disadvantage is that they may ice or fog up. The glasses produced over the last 4-5 years have proper ventilation making the icing and fogging problem a minor one. Most skiers now use such glasses during training and competition, even in less cold surroundings.
Contact lenses are worn by some athletes but it takes time to adjust to them and by their nature they may cause problems.
A cap or band just above the eyebrows will prevent sweat coming down to the eyes and irritating them. A doctor should see every athlete who has eye problems. Dark glasses may diminish photophobia - lesions are usually reversible. (2,6,13,17,18).
Hypothermic lesions in other organs.
Severe hypothermia (below 30/32 degrees C) may lead to bleeding in the mucosa of the small intestine, the stomach, the peritoneum and in subcutaneous tissues.
Subcutaneous bleeds are easily detected; bleeding in the abdomen may lead to mild or more severe constant or colic-like pain. Following severe gastrointestinal bleeds haematemesis (the vomiting of blood, which may be fresh or dark) and melaena (dark motions containing changed blood) may occur. The loss of large (or of multiple smaller) amounts of gastrointestinal content may lead to high blood viscosity, and in rare but extremely severe cases disseminated intravascular coagulation may be seen.
Increased frequency of overuse injuries and acute soft tissue injuries
In low temperatures muscles, tendons and joints may become “stiff and slow”. This may lead to an increased frequency of acute soft tissue injuries such as minor ruptures in muscles and tendons and distensions of ligaments and joint capsules.
The frequent occurrence of overuse injuries like tendonitis, periostitis, synovitis, bursitis etc is well known.
The importance of doing a proper warm up in low temperatures cannot be over estimated.
Skin lesions
The exposed portions of the body are most susceptible to frostbite - nose, lips, ears and face. Other peripheral portions of the body including fingers, toes, front of knees and shoulders, and the external genitalia of men are also often at risk. At first the skin becomes pale due to constriction of the blood vessels. Later a reddish area appears due to local hyperaemia, followed by oedema and numbness. With severe hypothermia, bullae (blisters) appear overlying deeper areas of necrosis which may require excision and skin grafting. (1,2,6,11.12,19).
Children exercising at low temperatures
Children are considerably more vulnerable than adults to the effects of cold and the lethal effect of hypothermia occurs earlier. Children have a greater surface area relative to their body weight and lose heat more rapidly. An adult with a height of 175 cm has a surface area of 280 cm2 per kilo body weight. A child with a height of 130 cm has a surface area of 330cm2/kilogram – i.e. a 25% greater surface area from which to lose heat. Because of the increased number of sweat glands per surface area in children they also lose more heat than adults. This must be taken into account when planning competitions and training for children in cold temperatures. For these reasons the temperature limits for competitions for children in cold climates must be above (i.e. warmer) than those by adults. Most authors having dealt with this problem recommend minus 12 degrees C as the lowest limit.
Treatment
Mild hypothermia:
The patient is brought into a warm room, given warm drinks, changed into warm clothes and covered with blankets.
Moderate hypothermia:
A patient with moderate hypothermia and a temperature between 34-30 degrees C must be resuscitated by gradually rewarming in a warm bath initially at a temperature of 26 degrees increasing to 42 degrees over a period of 7-8 minutes. The patient should be encouraged to drink warm fluids and if possible warm moisturised air should be inhaled.
Moderate and severe hypothermia may be exacerbated by after-drop i.e. the core body temperature may continue to fall even when the patient has been removed from cold to warmer area. Hayward and Steiner report promising results using a central rewarming technique when the patient breathes warm air and oxygen. It appears to be more effective in decreasing the effect of after-drop than rewarming in a bath from 26-40 degrees C.
Severe hypothermia:
A patient with severe hypothermia, with fixed dilated pupils, impalpable pulses, unrecordable blood pressure and with a core temperature below 30 degrees C should be taken to hospital as soon as possible. This should preferably be by helicopter - certainly the fastest means of transportation should be established as soon as possible from the arena or the training field. Cardiac monitoring should be established because of the dangers of cardiac arrhythmias and cardiac arrest. (7,8,11,16,17).
Rapid central rewarming by humidified oxygen and warm air using a breathing bag should be started. Cardiac massage and defibrillation are normally not necessary if the core temperature is above 30 degrees. Severe arrhythmias generally occur between 26 and 29 degrees C.
It may be necessary to treat patients with severe hypothermia by means of a heart-lung machine. In this way rewarming under proper cardiovascular control is possible in the most severe cases of hypothermia.
The patients should be handled as gently as possible to avoid precipitating ventricular fibrillation. A thermometer that can record down to 18 degrees C should be available. Intraoesophageal and rectal electronic thermometers are more accurate and reliable.
A few authors have reported survival in cases when a core body temperature as low as 19 degrees C has been recorded (16,17). Others cite survival when the body core temperature has been between 20-25 degrees C, but only in previously healthy individuals. (6,8,11).
Hypothermic accidents should not occur in either organised or recreational sports. In the event of over-exposure to cold a routine first aid procedure should be implemented. (9,11,16,17,18,19).
Summary:
Most winter and some summer sports take place in weather conditions which may lead to hypothermia. This may be due to simply to low temperatures, but may be aggravated by the humidity or the wind-chill effect. The lowering effect of the wind on temperature must not be ignored by organisers of winter competitions.
A summary of sign and symptoms follows.
Core Temperature - Signs and Symptoms
36-35 degrees C: Shivering, sensation of cold
35-33 degrees C: Violent shivering, sluggish thinking, poor coordination with loss of hand control, confusion, mood changes, pale skin with reddish or pink areas.
33-30 degrees C: Shivering replaced by muscular rigidity, confusion, semiconciousness, dilated pupils.. Later bullae and open wounds will develop
30-29 degrees C: Stupor, rigidity, slow pulse and respiration. The peripheral portion of the limbs, head and unprotected parts of the body will have obvious signs of local lesions such as bullae, open wounds, necrotic areas (depending on the lapse of time).
28-26 degrees C: Coma, arrhythmias, unrecordable pulse and blood pressure, shallow respiration. Cardiac monitoring is necessary, ideally with an ECG to detect ventricular fibrillation. If VF occurs it must be treated rapidly and adequately or death will ensue.
Conclusions:
Sports doctors, trainers, and all those responsible for the health of athletes must emphasise the
dangers of accidental hypothermia. The athletes themselves must learn to recognise weather
conditions that may lead to hypothermia. They must be made aware that shivering indicates that
heat loss is exceeding heat production, and also understand that loss of judgement and hand
coordination will inevitably follow uncontrollable shivering. They must be made aware that
tragedies caused by cold result from failure to respect prevailing weather conditions.
Recommendations:
- Gradual adaptation to training in cold climate is necessary.
- Consideration of the potential risk of cold-related problems is particularly important when travelling to international competitions because weather conditions may vary widely between different countries.
- Special attention must be paid to the increased risk of hypothermia in children
- Proper clothing with an inner temperature insulating layer and also an outer wind protective layer must be worn.
- During sports participation at low temperatures extra protection must be provided for the face, the front of the body, and the hands and feet.
- Special attention must be given to the eyes.
- Early change into dry clothes is essential.
- Pressure from the press and sponsors for interviews and photographs of the athletes at the site of the competitions may need to be countered in the interests of the athletes.
- NB. The health of the athlete is the most important factor.
- Doping control facilities must be comfortable, and the athletes must be given the opportunity to change into dry warm clothing.
- The waiting room for doping control should be well ventilated and warm.
- Warm drinks must be available immediately.
Recommended temperature limits.
- Long distance races (30 km and more) minus 16 degrees C.
- Shorter distances (below 30 km) minus 18 degrees C.
- Sprint races minus 20 degrees C.
- Temperature limits for children less than 14 years: minus12 degrees.
- High speed competitions such as alpine skiing, speed skiing and ski jumping should not take place below minus 20 degrees (the wind-chill effect is increased – even though with a relatively short time of exposure).
- Every sporting competition must take into consideration the fact that wind will increase the danger of hypothermia by effectively lowering the temperature.
Inggard Lereim
Vice-Chairman FIS Medical Committee
(Professor MDPhD,Univ.Hospital,Oslo)
May 2007
References
1. Bangs CC, Hamlet MP, Mills WJ,: Help for victim of hypothermia. Patient Care 11:46.15.12.1987.
2. Clothier JG Medical aspects of work in Arctic areas. Practitioner 213:805,1988.
3. Haywars JS, Steinmann AM: Accidental Hypothermia: An experimental study of inhalation rewarming. Aviat Space Environ med 46:1236,1995.
4. Guleria,JS, Talwar JR et al. Effect of breathing cold air on pulmonary mechanics in normal man. J.Appl.Physiol.1989 27(3),320-323.
5. Josenhans WT, Melville GN,Ulmer WT.The effect of facial cold stimulation on airway conductance in healthy man. Can.J.Physiol.Pharmacol 1979. 47,453-457.
6. Lane AM Cold injuries. Frostbite and hypothermia. Am.Coll.Surg 23:200.2003
7. Lassvik C Angina pectoris in cold. Linkjøping University, Sweden. Dissertation 1979,67
8. Leon CF et al. Left heart work and temperature responses to cold exposure in man. Amer.J.Cardiol.1970,26,38-45.
9. McFadden ER, Ingram RH. Exercise induced asthma. Observations on initiatory stimulus. N.Engl.J.Med 1979,301:14 363-379
10. Meriwether WD, Goodman RM: Severe accidental hypothermia with survival after rapid rewarming. Am J Med 53:505,1982
11. Miller JS, Nairn JR Cold air and ventilatory function. Brit J Dis Chest 1965,59,23-27.
12. Roach JJ, Kumagai R: Snowshoers hike higher, peri up too. Phys Sportsmed 4:30,1976 and 544 .2004.
13. Simonson,BG, Jacobs FM, Nadel JA. Role of autonomous nervous system and the cough reflex in increased responsiveness of airways in patients with obstructive airways disease. J.Clin.Invest.1967,46:1812-1818.
14. Strauss RH et al. Enhancement of exercise induced asthma by cold air. N.Engl.JU.Med.1987.,297:743-747.
15. Truscott DG, Firor WB, Clein LJ: Accidental profound hypothermia: Successful Resuscitation by core rewarming and assisted circulation. Arch Surg 106:216,1984 and 98:164 2005.
16. Severe accidental hypothermia. Lancet 1:237,1982
17. The Olympic BOOK of Sports Medicine 1994. Hypothermia and sports. Vol 1.
18. Advanced Trauma Leaders Course and manual 2006. American College of Surgeons.
19. F.I.M.S. Recommendations to Sports Medicine .2005.
